Secondary prevention of coronary heart disease ⋆ Treatment of the Heart. Prevention of coronary heart disease Coronary heart disease treatment and prevention
Chronic heart disease in Lately are being diagnosed more and more often, and not only among elderly patients. The occurrence of these pathologies is influenced by many factors: smoking, frequent stress, lack of physical activity and others. Unfortunately, only timely seeking help from a doctor can avoid the development of negative consequences.
International Classification of Diseases (ICD 10)
Heart disease is classified as the ninth class of pathologies of the circulatory system. It should be noted that this classification is a specially developed document that is used as the leading statistical basis in healthcare. The ICD is periodically revised under the guidance of WHO.
The ninth class also includes the following pathologies: ischemia (IHD), chronic rheumatic heart disease, cerebrovascular pathologies, lesions of veins/lymph nodes and others.
Even in the 20th century, mortality rates from diseases changed. If previously various types of infections acted as the cause of death, now they have been replaced by cardiovascular pathologies, injuries and cancer. For example, chronic rheumatic heart disease ranks next after arterial hypertension, stroke and coronary artery disease. However, in this article we will talk in more detail about the latest pathology, its causes of development, clinical forms and modern treatment methods.
general information
Coronary heart disease is a series of ailments characterized by insufficient blood supply of oxygen to the main muscles of the body. The development of this pathology is based on the constant process of deposition of atherosclerotic plaques on the walls of the coronary vessels. They consistently reduce the lumen of the arteries, thereby causing problems with the flow of blood to the heart and its normal functioning. Atherosclerotic deposits are also dangerous because they can self-destruct over time. Their fragments, along with the blood, are carried throughout the body. This is exactly how the well-known blood clots are formed.
In developed countries today, coronary heart disease is becoming the main cause of death and disability among the population. This pathology accounts for about 30% of deaths. According to available information, the disease is diagnosed in every third woman and almost half of men. This difference is very easily explained. Female hormones are a kind of protection against atherosclerotic vascular damage. However, when hormonal levels change, which is most often observed during menopause, the likelihood of developing the disease in the fair sex increases several times.
Classification
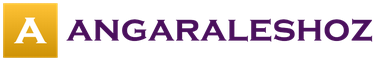
Back in 1979, a group of WHO specialists presented a classification of coronary heart disease. Symptoms, treatment and prognosis of each type has its own distinctive features.
- Asymptomatic form. Oxygen deficiency does not in any way affect the human condition.
- Angina (stable, unstable, spontaneous). This form manifests itself in the form of chest pain after physical activity, eating or a stressful situation.
- Arrhythmic form. It is accompanied by repeated interruptions in heart rhythm and often progresses to a chronic stage.
- The so-called coronary death. Complete cardiac arrest due to a sharp decrease in the level of blood entering the organ. This pathology occurs due to blockage of a large artery, which very often accompanies heart disease.
- Myocardial infarction. Characterized by the loss of a section of the heart muscle after prolonged oxygen deprivation.
The following subclasses are distinguished in angina pectoris:
- FC-1. Painful discomfort appears in response to severe physical activity.
- FC-2. Attacks occur when walking, after the next meal.
- FC-3. Pain occurs only after light exertion.
- FC-4. Manifests itself during the most minor emotional upheavals.
Causes
The most common disease leading to a consistent decrease in the lumen of blood vessels is considered to be atherosclerotic heart disease. With this pathology, the inside of the vessels is covered with a layer of fatty fragments, which subsequently harden. As a result, there is a difficulty in the flow of blood directly to the heart muscle itself.

Another cause of IHD is the so-called arterial hypertension. A decrease in blood flow initially entails the appearance of pain during physical activity (the required amount of oxygen is not supplied to the myocardium due to barriers to the blood flow), and then discomfort accompanies a person even in a calm state.
Atherosclerosis is very often the basis for the development of other pathological reactions. Among them greatest distribution received the following: spasm of the coronary arteries, the formation of blood clots, problems with diastolic-systolic function.
Factors contributing to the formation of ischemic heart disease
- Hereditary predisposition.
- High cholesterol levels.
- Bad habits (tobacco smoking, alcohol abuse). Smoking cigarettes has been reported to increase the risk of developing various forms coronary heart disease by 6 times.
- High blood pressure.
- Obesity.
- Diabetes.
- Complete absence of sports activities, sedentary work.
- Old age (many heart and vascular diseases develop after 50 years).
- Excessive consumption of fatty foods.
- Frequent stress. They certainly increase the load on the heart, blood pressure increases, which impairs the delivery of oxygen to the main organ.
The causes and rate of formation of ischemia, its severity and duration, the initial state of health - all these factors predetermine the appearance of one or another form of coronary heart disease.
Symptoms
Treatment of this pathology is prescribed only after the appearance of its first signs, as well as a complete diagnostic examination. What symptoms are characteristic of IHD?

All of the above factors are a clear sign that the patient has coronary heart disease. Symptoms, of course, may vary in each specific case and differ in intensity. What signs characterize certain forms of IHD?
Deterioration of blood flow in the coronary vessels when the lumen is completely closed by a thrombus can lead to acute ischemia, in other words, to myocardial infarction, and if it is partially closed, to chronic oxygen starvation of the heart, and this is angina. Both acute and chronic versions of ischemia are accompanied by pain in the chest area.
With a heart attack, this type of discomfort occurs suddenly. These are usually short-term attacks. Gradually their intensity increases, literally after an hour the pain becomes unbearable.
With angina, the main symptom is chest discomfort that occurs during intense physical or emotional stress. The duration of the attack itself, as a rule, does not exceed 2-3 minutes. At the initial stage of development of the pathology, the patient feels pain in the sternum, and as the disease develops, the intensity increases. During the next attack, difficulty breathing and fear appear. Patients stop moving and literally freeze until the attack finally stops.
In addition to the common forms of angina, there are types of coronary heart disease in which the symptoms described above are either mildly expressed or completely absent. Instead of severe pain, patients may experience attacks of suffocation, heartburn, and weakness in the left arm.
Sometimes painful discomfort is localized exclusively in the right side of the chest. In some cases, the disease makes itself felt during reading or during normal housework, but does not appear during sports or emotional stress. As a rule, in this case we are talking about Prinzmetal's angina. This type of pathology, according to experts, is characterized by an individual cyclical occurrence of attacks; they occur exclusively at a certain time of the day, but most often at night.
Recently, so-called silent coronary heart disease has become increasingly common. Its treatment, as a rule, is complicated by the fact that it is not possible to carry out the necessary diagnostic operations in a timely manner. In this kind of situation, therapy is prescribed in the later stages.
Diagnostics
Pathology such as coronary heart disease should not be ignored. The symptoms described in this article should alert you and be a reason for everyone to consult a specialist.
At the appointment, the doctor first collects a complete medical history of the patient. He may ask a number of clarifying questions (when the pain began, its nature and approximate location, whether close relatives have similar pathologies, etc.). IN mandatory A diagnostic examination is prescribed, which includes the following procedures:

To finally determine the causes of coronary heart disease, an additional study of the level of cholesterol, triglycerides, lipoproteins, and blood sugar may be required.
What should the therapy be like?
The tactics of combating various clinical forms of the disease have their own characteristics. However, it is necessary to identify the main directions that are actively used in modern medicine:
- Not drug treatment.
- Therapy using medicines.
- Carrying out coronary artery bypass grafting.
- Help from endovascular techniques (coronary angioplasty).
Non-drug therapy involves lifestyle and nutrition adjustments. For any manifestations of coronary artery disease, a strict limitation of the usual mode of activity is indicated, since during physical activity there is often an increase in the myocardial oxygen demand. Its dissatisfaction, as a rule, provokes coronary heart disease of this nature. That is why, in any clinical form of IHD, the patient’s activity is limited, but during the rehabilitation period it gradually expands.
Diet for illness involves limiting the consumption of water and salt to reduce pressure on the heart muscle. If the cause of the pathology is hidden in obesity, or atherosclerotic heart disease is to blame, a low-fat diet is recommended. It is necessary to limit the consumption of the following products: lard, fatty meat, smoked meats, baked goods, chocolate, baked goods. For supporting normal weight It is important to constantly monitor the balance of energy consumed and expended.

Drug therapy is based on taking the following groups of drugs:
- Antiplatelet agents (Aspirin, Thrombopol, Clopidogrel). These drugs are responsible for reducing blood clotting.
- Anti-ischemic drugs (Betoloc, Metocard, Coronal).
- ACE inhibitors to lower blood pressure (Enalapril, Captopril).
- Hypocholesterolemic drugs responsible for reducing cholesterol levels (Lovastatin, Rosuvastatin).
Some patients are additionally prescribed diuretics (Furosemide) and antiarrhythmics (Amiodarone). Sometimes even competent drug therapy does not help in the fight against such pathologies as coronary heart disease. Treatment through surgery is the only correct solution in this situation.
As a rule, coronary artery bypass grafting is recommended. This operation is used to provide the heart with oxygen and restore its normal functioning. The patient's own blood vessels are used as a new path of blood flow, which are moved directly to the heart and then sutured. This operation relieves the patient of possible attacks of angina pectoris, reduces the risk of sudden cardiac death and the development of a heart attack.
Minimally invasive techniques include coronary angioplasty. During this operation, a special stent frame is installed in the narrowed vessel, which holds the vessel lumen sufficient for normal blood flow.

Other treatment methods
- Hirudotherapy. This treatment method is based on the use of the antiplatelet properties of leech saliva. Currently, in our country this approach is used extremely rarely and only at the request of the patients themselves. The only positive result of hirudotherapy is considered to be the prevention of blood clots.
- Use of stem cells. It is assumed that after stem cells are introduced into the body, they differentiate into the missing components of the myocardium. Stem cells do have this ability, but they can transform into any other cells in the body. Despite the positive results this method treatment, it is not used in practice today. In many countries, this technique is experimental in nature and is not included in the accepted standards of care for patients with coronary artery disease.
Possible complications
The most dangerous complication of various forms of coronary heart disease is considered to be the occurrence of an attack of acute failure, which often leads to death.
In this condition, death occurs instantly or within six hours after the immediate onset of a painful attack. According to experts, 70% of deaths are caused by this complication in the presence of predisposing factors (alcohol intake, heart rhythm disturbances, myocardial hypertrophy).
The risk group also includes patients who do not receive proper therapy for this diagnosis.
Other equally dangerous complications of coronary artery disease include the following: myocardial infarction (in 60% of cases the problem is preceded by another pathology called angina pectoris), heart failure.
How to prevent the development of the disease?
What should be the prevention? Heart diseases are mostly caused by proper nutrition. That is why experts strongly recommend that you first completely review your usual diet. It should be as balanced as possible and consist exclusively of “healthy” foods. Food sources of cholesterol should be excluded from the diet and saturated fat(fatty meat, sausages, lard, dumplings, mayonnaise). Fresh fruits, vegetables, herbs, seafood, nuts, mushrooms, cereals, legumes - all these are components of proper nutrition. They are safe for patients with primary signs of coronary artery disease.
The human heart is a rather complex organ that requires appropriate attention. As you know, its work is significantly deteriorated if a person is overweight. That is why, in order to prevent the development of coronary artery disease, it is recommended to keep body weight under constant control. Should be arranged periodically fasting days and monitor your caloric intake.

Doctors recommend regular physical activity to everyone without exception. There is no need to go to the gym every day or start playing serious sports. Hiking, yoga, therapeutic exercises - such simple activities can radically improve your health and prevent coronary heart disease. Prevention of the disease also means reducing stress and completely giving up bad habits. As is known, it is the latter that not only contribute to the development of IHD, but also significantly complicate the quality of life of a person and his immediate environment. As for stress, avoid it by Everyday life extremely difficult. In this kind of situation, experts recommend changing your attitude to everything that is happening and starting to do breathing exercises.
Conclusion
In this article, we have explained in as much detail as possible what coronary heart disease is. Symptoms, treatment and causes of this pathology should not be ignored, since they are all interconnected. Timely consultation with a doctor and full compliance with all his recommendations allow you to control coronary artery disease, as well as prevent the occurrence of various types of complications. Be healthy!
Prevention of coronary heart disease in clinical practice
In 1998, the recommendations of the second joint working group of the European Society of Cardiology, the European Society of Atherosclerosis and the European Society of Hypertension “Prevention of coronary heart disease in clinical practice” were published in the journals “European Heart Journal”, “Atherosclerosis” and “Journal of Hypertension”. These data will undoubtedly be of interest to the general medical community.
The main idea of the recommendations is to concentrate the efforts of therapists, cardiologists, and general practitioners on reducing the risk of developing coronary heart disease (CHD) and its complications, as well as other clinical manifestations of atherosclerosis. The goal is to ensure that the prevention of coronary artery disease becomes an integral part of the treatment and preventive work of a practicing physician. Doctors still pay a lot of attention to the treatment process and do not make sufficient use of the enormous potential that
laid down in the prevention of coronary artery disease. Main principle: IHD is a multifactorial disease, so assessment of the risk of its development and prevention must be multifactorial.
A key element of patient management is the need to achieve target levels of blood pressure and blood lipids as the main factors determining the risk of developing coronary artery disease and its complications. To achieve target levels, it is recommended as lifestyle changes (diet, physical activity, smoking cessation), as well as the use of lipid-normalizing and antihypertensive medications.
The relationship between drug and non-drug methods and patient management tactics are determined by the level of absolute multifactorial coronary risk. This risk is expressed in the form of the likelihood of clinical manifestations of ischemic heart disease, atherosclerotic lesions of other localization or their complications in
over the next 10 years. Absolute individual risk is determined by five main indicators: age, gender, smoking, systolic blood pressure and total cholesterol, taking into account heredity, changes in the lipid spectrum, and the presence of diabetes. Patients with existing symptoms of coronary artery disease or other atherosclerotic lesions are at very high risk.
Medical priorities. Against the background of well-known general recommendations to reduce smoking, choose a healthier diet, and increase physical activity, addressed to the entire population as part of a population-based prevention strategy, the target group for the implementation of the proposed medical approach are patients with clinical manifestations of coronary artery disease, atherosclerotic lesions of other localization or a high risk of them development. Patients with the greatest risk receive the greatest benefit from preventive measures. In accordance with this, the following target groups are identified, arranged in descending order of priority:
1. Patients with coronary artery disease or other
diseases associated with atherosclerosis (AS).
2. Healthy individuals at high risk of developing IHD and other diseases associated with AS, due to a combination of risk factors such as smoking, elevated blood pressure, lipid metabolism disorders (increased levels of total cholesterol and low-density lipoprotein cholesterol (LDL-C) , decreased levels of high-density lipoprotein cholesterol (HDL-C) and increased levels of triglycerides), increased blood sugar, a family history of early development of coronary artery disease, and persons with severe hypercholesterolemia (or other forms of dyslipidemia), hypertension or diabetes mellitus.
3. Close relatives of patients with early development of coronary artery disease or other diseases associated with AS, as well as healthy individuals at very high risk.
4. Other persons (patients) undergoing examination as part of routine clinical practice.
Measures for the first group of patients are outlined in the section “Secondary prevention”, in relation to
other groups - in the “Primary Prevention” section.
Secondary prevention. Lifestyle changes. Success in this direction is determined by the patient’s readiness to change his lifestyle. The moment a patient is diagnosed with coronary artery disease or a high risk of its development provides him with an ideal opportunity to reconsider his lifestyle, and the doctor’s advice falls on favorable ground.
To give up smoking. The doctor should recommend that the patient stop smoking in order to preserve health and life, inform him about the dangers of passive smoking, while relying on the help of family members. In some cases, at the first stage of quitting smoking, nicotine replacement therapy may be useful, especially in cases of severe nicotine addiction. Stopping other family members who live in the same room as the smoker from smoking can help the smoker quit and avoid taking up the habit again.
Changing your diet:
1. Reduce total fat consumption to 30% or less of the total calorie intake; saturated fat to one
a third or less of all fat consumed; cholesterol up to 300 mg per day. Considering the nutritional pattern of the urban population of Belarus, it is necessary to increase the consumption of fish and other seafood.
2. Increase consumption of fresh vegetables, fruits and grain products.
3. Reduce the total calorie content of the daily diet if you are overweight.
4. Reduce salt and alcohol intake if blood pressure is high.
Increasing physical activity. Aerobic exercise (walking, swimming, cycling) is recommended for 20^0 minutes 4^ once a week. It is important that physical exercise increases the level of high-density lipoproteins (anti-atherogenic), reduces the content of triglycerides, the likelihood of thrombosis, and helps normalize weight.
Overweight and obesity. To assess body weight and identify obesity, the body mass index (BMI) is used, which is calculated using the formula: weight in kg/(height in m2).
Persons with overweight (BMI>25 kg/m2) and obesity (BMI>30 kg/m2), especially with
central type of obesity have an increased risk of coronary artery disease, therefore, to lose weight they should be provided with professional help based on an appropriate diet and increased physical activity. Losing weight will also help lower blood pressure, total cholesterol and blood sugar levels. Waist circumference is often used as a clinical indicator of obesity and weight loss monitoring. A waist circumference of >94 cm in men and >80 cm in women indicates that extra pounds should be lost, and if the waist circumference is >102 cm in men and >88 cm in women, a professional blood pressure test is required. The need to achieve and constantly maintain a target blood pressure level of less than 140/90 mmHg is emphasized. If lifestyle changes cannot achieve this level of blood pressure, antihypertensive drugs should be prescribed. In patients with exertional angina, preference is given to p-blockers, and if they are intolerable or insufficiently effective, calcium channel blockers are given to prolonged release.
bathroom action. It is advisable to prescribe β-blockers to patients with a history of myocardial infarction, and ACE inhibitors to patients with left ventricular dysfunction.
Blood lipids. The level of total cholesterol must be consistently reduced to 5.0 mmol/l (190 mg/dl) and below, and LDL-C to 3.0 mmol/l (115 mg/dl) and below. Formally, the levels of HDL-C and triglycerides are not considered as criteria for the effectiveness of treatment, but the level of HDL-C<1,0 ммоль/л (40 мг/дл) и триглицеридов >2.0 mmol/L (180 mg/dL) is an indicator of an increased risk of developing CHD.
If LDL-C levels cannot be consistently maintained through lifestyle changes, drug treatment should be considered. Preference should be given to HMG coenzyme-A reductase inhibitors (statins), since this class of lipid-normalizing medications has demonstrated undeniable effectiveness in reducing coronary and overall mortality and increasing life expectancy. Statins also significantly reduce the risk of stroke in
patients with ischemic heart disease.
Blood sugar. It has not yet been established to what extent blood sugar control reduces the risk of cardiovascular complications in patients with diabetes and coronary artery disease, but normoglycemia is known to help prevent micro- and macrovascular complications in people with diabetes. For type 1 diabetes (insulin-dependent diabetes mellitus), the following target levels should be achieved:
fasting blood sugar - 5.16.5 mmol/l (91 - 120 mg/dl);
blood sugar after meals (peak level) - 7.69.0 mmol/l (136-160 mg/dl);
glycosylated hemoglobin (HbA) - 6.2-7.5%.
In addition, hypoglycemia should be avoided.
For most patients with type 2 diabetes (non-insulin-dependent diabetes mellitus), lower levels of these indicators should be achieved. For some patients, especially the elderly, extreme caution should be exercised in achieving target levels.
Other preventive drug therapy. IN
In addition to non-drug and drug control of blood pressure and blood lipids, it is necessary to take into account the advisability of prescribing drugs to patients that reduce the risk of complications and mortality:
Aspirin (at least 75 mg/day) or other drugs that affect platelet aggregation, if possible, in all patients.
β-blockers - for patients who have had a myocardial infarction.
ACE inhibitors - for patients with decreased left ventricular systolic function (ejection fraction< 40) или тем, у кого в период острого инфаркта миокарда были симптомы сердечной недостаточности.
Anticoagulants - for patients after myocardial infarction with an increased risk of thromboembolic complications, including patients with extensive anterior myocardial infarction, left ventricular aneurysm or thrombosis, paroxysmal tachyarrhythmia, chronic heart failure and a history of thromboembolism (under the control of prothrombin and other indicators of hemostasis).
Primary prevention.
The first step is the determination of coronary risk, which is made using a special map (Fig. 1, see the paper version of the journal).
To determine the absolute risk of clinical manifestations of coronary artery disease in the next 10 years, you should select a table for the desired gender and its part corresponding to the age and smoking status (smoker, non-smoker) of this person. Then you need to find the cell closest to his or her systolic blood pressure and cholesterol level, and compare the shading of that cell with the scale at the bottom of the diagram. The charts help you evaluate the impact that changes in cholesterol levels, blood pressure, or smoking status may have on your overall risk. Moving along the tables (diagrams) to the right, you can trace the influence of long-term (over decades) action of the risk factor. This can be helpful when discussing the issue with younger people. In patients with diabetes mellitus, familial hyperlipidemia, reduced HDL-C levels (<1,0 ммоль/л у мужчин и <1,1 у женщин), имеющих прямых родственников с
early ischemic heart disease (men under 55 years of age, women under 65 years of age), the risk increases by one category compared to that determined by the map. The criterion for high risk is its level of >20% or, extrapolated to age 60 years, a risk of >20% in the next 10 years.
For patients whose coronary risk is assessed as high, intensive measures to reduce risk factor levels using medications as indicated are recommended.
Lifestyle. Individuals at high risk of developing CHD especially need professional support in quitting smoking, making healthy nutritional choices, and increasing physical activity. In primary prevention, importance is attached to preventing obesity and reducing excess weight. Lifestyle changes may help avoid drug treatment. The lifestyle recommendations for patients with coronary artery disease outlined above may also be useful for individuals at high risk for this disease.
Arterial pressure. It is emphasized that the achievement
Targeted blood pressure levels significantly reduce the likelihood of stroke, myocardial infarction, and heart failure in these patients. The decision to use antihypertensive medications is based both on an assessment of absolute coronary risk and on the level of systolic and diastolic pressure and the presence of target organ damage (Fig. 2, see the paper version of the journal).
For patients with an increase in systolic blood pressure (SBP) >180 mm Hg and/or diastolic blood pressure (DBP) > 100 mm/Hg, persisting despite changes in lifestyle, the risk of complications (coronary artery disease, cerebral stroke, heart failure) is so high that drug treatment is required. Drug treatment is also necessary for those patients whose SBP is consistently maintained at a level of 160 - 179 mmHg. Art. In individuals with a more moderate increase in blood pressure (SBP 140 - 159 and/or DBP 90 -94 mm Hg), drug treatment is prescribed for target organ damage or a high risk of coronary artery disease. If at the same blood pressure levels the absolute risk
is low, you can do without medications.
When carrying out therapy aimed at lowering blood pressure, it is necessary to determine the target level of reduction and titrate the dose of the drug until the goal is achieved. It is preferable to start treatment with one drug. If necessary, a second or third drug can be added. As part of primary prevention, the target level of blood pressure reduction is 140/90 mmHg. and below. In young people, patients suffering from diabetes mellitus and renal parenchymal diseases, the target blood pressure level may be even lower.
The effectiveness of diuretics and beta-blockers in reducing morbidity and mortality from cardiovascular disease in people with hypertension is well established. Similar effectiveness has recently been identified for calcium antagonists and ACE inhibitors. Therefore, to adequately control blood pressure, antihypertensive drugs of various classes can be used with equal success.
Blood lipids. The decision to use lipid-lowering drugs depends on the
absolute risk of developing CHD, lipid levels and cases of early development of CHD or other diseases associated with atherosclerosis in the family (Fig. 3, see the paper version of the journal). Patients with familial hypercholesterolemia have such a high risk of developing coronary artery disease that drug treatment is always necessary. In other cases, the tactics are determined by the level of coronary risk. If the risk is more than 20%, total cholesterol, HDL-C (a-cholesterol), triglycerides, and LDL-C are determined. You should follow a lipid-lowering diet with repeated monitoring after 3-6 months. If it is not possible to reduce LDL cholesterol to 3.0 mmol/l (total cholesterol to 5.0 mmol/l), lipid-normalizing drugs are prescribed against the background of constant adherence to a lipid-lowering diet. When using lipid-lowering drugs, it is necessary to titrate the drug dose until the target level of cholesterol reduction is achieved. Sometimes, in individuals at high risk for developing CAD, target levels of lipid reduction cannot be achieved either by diet or by the maximum dose of lipid-lowering medications; V
In this case, combined drug treatment is required. Even in those patients who have very high levels of total cholesterol or LDL-C and fail to achieve the target level of lipid reduction, the risk of developing coronary artery disease can be significantly reduced. The drugs of choice may be medications of four main groups (statins, fibrates, niacin, bile acid sequestrants), however, evidence of the effectiveness and safety of statins is most demonstrative in primary prevention.
Blood sugar. There is currently no data on the effectiveness of blood sugar control in reducing the risk of developing coronary artery disease or other AS-related diseases in patients with diabetes. However, in people with both types of diabetes, the risk of developing diseases associated with AS directly depends on the degree of hyperglycemia. Control of blood sugar levels (as determined for patients with coronary artery disease) contributes to the effective prevention of microvascular disease and other complications associated with diabetes, so it is advisable to achieve adequate reduction in blood sugar levels in all individuals with diabetes.
blood sugar. At any level of risk factors (smoking, blood pressure, blood lipids) or any combination of them, the absolute risk of developing coronary artery disease is much higher in patients with diabetes than without it. Therefore, it is important to achieve targeted reductions in risk factor levels in patients with diabetes.
Examination of close relatives. In close relatives of patients suspected of having familial hypercholesterolemia or other hereditary forms of dyslipidemia, blood lipid levels should be determined.
Prepared by G.I. SIDORENKO, IL KOZLOV (Belarusian Research Institute of Cardiology)
Medical news. - 2000. - No. 8. - pp. 34-38.
Healthcare in Norway
At the beginning of the 21st century. Norway is an example of a modern democracy where society as a whole is responsible for the well-being of each citizen. On an area of about 400 thousand square meters. km live 4.525 million people. Because of geographical features the population is distributed unevenly throughout the country: 2/3 live in densely populated areas, 1/3 -
in coastal areas of the Norwegian Sea. For many Norwegians, fishing is still the main source of income. However, in the mid-60s, oil fields were discovered in Norway, which marked the beginning of the growth and strengthening of the socio-economic well-being of citizens and the state as a whole. This was reflected in the average duration
Coronary heart disease is a serious problem. It is one of the most common causes of sudden death. Everyone should know the symptoms of this disease, since no one is immune from this disease. Prevention of coronary heart disease will help avoid the development of this disease.
Cardiac ischemia
Ischemia begins its development when the heart is insufficiently saturated with oxygen. It is accompanied by shortness of breath and pain. It is worth noting that this is the most common heart disease, which in its severe form can be fatal. Therefore, prevention of the disease should begin as early as possible, without waiting for its first symptoms.
The cause of the disease can be high blood pressure, high cholesterol. Alcohol and smoking are the enemies of a healthy heart. Frequent stress and exposure to depression can also lead to ischemia.
There are many reasons for the development of IHD; in order to prevent the development of the disease, it is important to know what can serve as an impetus for its onset.
Risk factors
Risk factors are predisposing causes that increase the likelihood of developing a disease or its exacerbation. Risk factors for coronary heart disease are divided into two groups. One of them includes inevitable causes that cannot be eliminated. Unavoidable factors for coronary heart disease include:
- age, people over 40 years of age are more susceptible to heart disease;
- gender, the risk group includes mainly men;
- heredity, the disease in most cases is inherited.
 The second group includes factors that can be regulated:
The second group includes factors that can be regulated:
- smoking;
- excess cholesterol in the blood;
- excessive alcohol consumption;
- obesity;
- sedentary lifestyle;
- high blood pressure.
To reduce the risk of developing the disease, it is necessary, if possible, to reduce or completely eliminate the factors included in the second group. This will significantly reduce the possibility of developing ischemia.
Types of prevention of coronary heart disease
 Prevention of IHD is expressed in two ways: primary and secondary prevention of IHD. In the first case preventive measures are aimed at eliminating the possibility of the occurrence of a disease such as coronary artery disease.
Prevention of IHD is expressed in two ways: primary and secondary prevention of IHD. In the first case preventive measures are aimed at eliminating the possibility of the occurrence of a disease such as coronary artery disease.
In the second case, preventive measures are aimed at avoiding exacerbation of an already formed disease.
This means that primary prevention of CHD is carried out by people who do not have coronary heart disease, and secondary prevention concerns those who already suffer from CHD.
Primary prevention
Primary prevention of IHD is carried out among healthy people. The main goal of this procedure is to prevent the disease and reduce risk factors for its development.
In case of coronary heart disease, prevention should begin with the organization of proper nutrition. Increased level Cholesterol in the blood is the cause of many cardiovascular diseases. You can control blood cholesterol levels with a special diet.
In some cases, cholesterol can be regulated with the use of drugs - statins. You also need to ensure that the glucose level in the blood is not exceeded.
 A special diet is one of the important points in the prevention of ischemia and deserves special attention.
A special diet is one of the important points in the prevention of ischemia and deserves special attention.
The principle on which a preventive diet for ischemic heart disease is based is to reduce the amount of fat, sugar, and salt in the diet. To do this, consider the following recommendations:
- limit or completely remove animal fats from the daily menu;
- eat fried foods as little as possible, or better yet, avoid them altogether;
- limit salt intake;
- do not eat a lot of eggs, it is enough to eat no more than two eggs per week;
- Do not overuse confectionery products;
- cereals are useful, especially those that have undergone minimal processing;
- increase intake of vegetables and fruits;
- replace meat with sea fish; ocean fish and fish oil are also equally useful.
With such a diet, the blood vessels will be reliably protected, and this is a good prerequisite for heart health.
It is important not to overindulge in high-calorie foods to prevent excess weight. The number of calories consumed should correspond to those expended.
 It is necessary to properly organize your daily routine. It should include time for daily physical activities. It is important to avoid overwork; a person needs proper rest and sleep. Stress and emotional overload worsen a person’s general condition and lead to heart disorders.
It is necessary to properly organize your daily routine. It should include time for daily physical activities. It is important to avoid overwork; a person needs proper rest and sleep. Stress and emotional overload worsen a person’s general condition and lead to heart disorders.
In addition, preventive measures should include the following:
- if the pressure is elevated, it needs to be normalized; in order to do this, you will need to consult a doctor;
- Heart diseases are much more common in people who smoke, so it is important to fight smoking;
- Excessive alcohol consumption, drinking strong coffee in large quantities increases the risk of developing the disease, these drinks need to be eliminated;
- Upon reaching 40 years of age, it is required to make a preventive visit to a cardiologist at least once a year.
With a responsible approach to business and following all recommendations for the prevention of coronary artery disease, the risk of developing the disease can be reduced several times.
Secondary prevention
Secondary prevention concerns individuals who have been diagnosed with coronary heart disease. In this case, all possible measures should be taken to prevent an exacerbation of the disease.
 Patients diagnosed with ischemia need to lead a correct lifestyle to prevent deterioration of their health.
Patients diagnosed with ischemia need to lead a correct lifestyle to prevent deterioration of their health.
Measures secondary prevention:
- compliance with all points included in primary prevention;
- prevention of spasms of coronary vessels with medicines;
- taking measures to prevent heart failure;
- treatment aimed at preventing and eliminating various types of arrhythmias;
- surgical measures that have to be resorted to in extreme cases.
Preventive measures for ischemia should include taking medications that will satisfy the myocardial oxygen demand. These medications include:
- acetylsalicylic acid;
- statins;
- beta blockers;
- ACE inhibitors.
Anyone who suffers from ischemia should have nitroglycerin in their first aid kit. It is used both in the treatment and prevention of ischemia.
 The action of the drug is aimed at improving the contractile function of the heart muscle and reducing its need for oxygen.
The action of the drug is aimed at improving the contractile function of the heart muscle and reducing its need for oxygen.
The listed procedures are aimed at eliminating exacerbations of the disease, improving the quality of life in the presence of a diagnosis of coronary heart disease, as well as preventing sudden death from an attack of coronary heart disease.
It is important that the patient takes his health seriously and responsibly and follows all the doctor’s recommendations.
Secondary prevention is carried out under the supervision of a doctor who will monitor the patient’s condition.
When to start taking preventive measures
Some preventive procedures can be started as early as childhood. It is important to ensure that a teenager does not start smoking at an early age. Smoking in itself, and especially at an early age, is a risk factor for the development of coronary artery disease.
 Rules healthy eating It is necessary to start vaccinating a child from an early age. This will subsequently save you not only from ischemic heart disease, but also from many other diseases.
Rules healthy eating It is necessary to start vaccinating a child from an early age. This will subsequently save you not only from ischemic heart disease, but also from many other diseases.
Beginning with adolescence, blood pressure should be monitored.
Thus, primary preventive work should begin as early as possible, teaching the child to healthy image life. People who have crossed the 40-year-old threshold should strengthen the prevention of ischemia, since at this age the risk of developing the disease is very high.
There are primary and secondary prevention of coronary heart disease.
Primary prevention of coronary heart disease consists of carrying out special measures before the onset of the disease (impact on risk factors to slow the progression of the atherosclerotic process).
Secondary prevention of coronary disease is carried out in the presence of an existing disease to prevent the progression of the disease and prevent subsequent complications. Currently, secondary prevention of IHD predominates, since primary prevention requires public policy on a healthy lifestyle.
Risk factors for coronary heart disease
Existing risk factors for coronary disease are divided into modifiable (modifiable) and non-modifiable (constant, non-modifiable).
Family history of coronary heart disease
The risk of developing coronary disease is increased:
- in close relatives of a patient with IHD (more important for first-degree relatives - parents, brothers, sisters, sons, daughters, than for second-degree relatives - uncles, aunts, grandparents);
- with a large number of patients with coronary artery disease in the family;
- when IHD occurs in relatives at a relatively young age.
Age
A linear relationship was revealed between age and signs of coronary heart disease (the older the age, the more pronounced atherosclerosis and the higher the incidence of coronary heart disease).
Up to 55 years of age, the incidence of coronary disease among men is 3-4 times higher than among women (with the exception of women suffering from arterial hypertension, hyperlipidemia, diabetes mellitus, and early menopause). After 75 years, the incidence of coronary heart disease among men and women is the same.
Smoking
Smoking increases the risk of developing coronary heart disease by 2 times. Smoking causes a transient increase in fibrinogen levels in the blood, narrowing of the coronary arteries, platelet aggregation, a decrease in HDL cholesterol levels in the blood, and an increase in the concentration of LHT cholesterol. In addition, substances contained in tobacco smoke can damage the endothelium and promote the proliferation of smooth muscle cells (ultimately forming foam cells). According to autopsy data, in smokers who died from causes unrelated to coronary heart disease, atherosclerosis of the coronary arteries is more pronounced than in non-smokers. Smoking cessation leads to a 50% reduction in the incidence of myocardial infarction in the population. However, smoking has a major effect on the incidence of sudden cardiac death.
Quitting smoking leads to a reduction in the risk of cardiovascular disease, which can reach the level for non-smokers within one year of abstinence.
Signs of arterial hypertension
High blood pressure (both systolic and diastolic) increases the risk of developing coronary artery disease by 3 times.
Diabetes
In type I diabetes mellitus, insulin deficiency leads to a decrease in the activity of LGOTases and, accordingly, to an increase in the synthesis of triglycerides. With symptoms of type II diabetes mellitus, there is type IV dyslipidemia with increased VLDL synthesis. In addition, diabetes mellitus is often combined with obesity and arterial hypertension.
Sedentary lifestyle
A sedentary lifestyle significantly increases the risk of developing CHD.
Obesity
Obesity predisposes to symptoms of dyslipidemia, hypertension and diabetes mellitus.
Estrogen deficiency in coronary heart disease
Estrogens have a vasoprotective effect. Before menopause, women have higher levels of LHT cholesterol, lower concentrations of LDL cholesterol, and a 10-fold lower risk of CHD than men of the same age. During menopause, the protective effect of estrogen decreases and the risk of coronary artery disease increases (which dictates the need to replenish estrogen from the outside).
Risk factor assessment
The presence of several risk factors leads to signs of an increase in the risk of developing coronary heart disease several times, and not simply to the summation of degrees of risk. When assessing the risk of developing coronary heart disease, the following parameters are determined:
- Unchangeable risk factors are age, gender, family history, and the presence of atherosclerotic manifestations.
- The patient’s lifestyle—smoking, physical activity, dietary habits.
- The presence of other risk factors - excess body weight, arterial hypertension, lipid and glucose levels in the blood.
To assess body weight, you can focus on such a sign as body mass index - the ratio of body weight (in kg) to body surface area (in m2).
Secondary prevention of coronary heart disease
Secondary prevention in a patient with coronary artery disease consists of changing lifestyle, influencing risk factors, and using JTC.
- Lifestyle change
- Stop smoking.
- Dieting.
- Reducing the consumption of animal fats to 30% of the total energy value of food.
- Reduce saturated fat intake to 30% of total fat.
- Cholesterol intake no more than 300 mg/day.
- Replacing saturated fats with polyunsaturated and monounsaturated fats of plant and marine origin.
- Increasing consumption of fresh fruits, plant foods, cereals.
- Limiting total calorie intake if you are overweight.
- Reducing salt and alcohol consumption with high blood pressure.
- Increase physical activity. The following physical exercises are recommended: brisk walking, jogging, swimming, cycling and skiing, tennis, volleyball, dancing with aerobic physical activity. In this case, the heart rate should be no more than 60-70% of the maximum for a given age. Duration physical exercise should be 30-40 minutes: 5-10 minutes warm-up, 20-30 minutes aerobic phase, 5-10 minutes final phase. Regularity: 4-5 times a week (for longer sessions - 2-3 times a week).
Impact on risk factors for coronary heart disease
If your body mass index is more than 25 kg/m2, you need to lose weight through diet and regular exercise. This leads to signs of decreased blood pressure, a decrease in the concentration of total cholesterol and LDL cholesterol in the blood, an increase in HDL cholesterol, an increase in glucose tolerance and insulin sensitivity.
For elevated blood pressure, antihypertensive drugs are prescribed if non-drug treatment has no effect. Blood pressure below 140/90 mmHg is considered optimal. Art.
In case of hypercholesterolemia or a complex form of dyslipidemia, it is necessary to reduce the concentration of total cholesterol to 5 mmol/l (190 mg%) and LHTDL cholesterol to 3 mmol/l (115 mg%) using dietary measures, and then using antihyperlipidemic drugs (especially in the presence of severe manifestations of ischemic heart disease). After myocardial infarction, the prescription of antihyperlipidemic drugs is recommended 3 months after its occurrence (the time necessary to stabilize blood lipid levels and evaluate the effect of dietary measures).
In the presence of symptoms of type I diabetes mellitus, the optimal glucose concentration is considered to be 5.1-6.5 mmol/l (91-120 mg%), the optimal peak glucose concentration is 7.6-9 mmol/l (136-160 mg%). Prevention of serious hypoglycemic conditions is also necessary. For patients with type I diabetes mellitus, lower blood glucose values are recommended.
Application of drugs
- Acetylsalicylic acid (minimum dose 75 mg).
- Beta blockers are necessary for patients after myocardial infarction (especially with complications during myocardial infarction in the form of arrhythmias), even in the absence of angina.
- ACE inhibitors are indicated for patients after myocardial infarction with signs of heart failure or left ventricular dysfunction.
- Anticoagulants are indicated for patients after myocardial infarction with an increased risk of thromboembolism.
Primary prevention of coronary heart disease
The absolute risk of developing coronary disease in the next 10 years can be assessed using special coronary risk maps developed by the International Societies for Coronary Prevention. To do this, it is necessary to determine such characteristics as age, gender, smoking habit, systolic blood pressure and total cholesterol concentration.
Primary prevention is carried out in individuals at increased risk of developing coronary artery disease. Measures for primary prevention of coronary artery disease consist of changing lifestyle and influencing risk factors. They are similar to the above measures for secondary prevention of coronary artery disease.
Prevention of ischemic
heart diseases
Prevention of coronary heart disease is a series of comprehensive measures aimed at preventing the onset of the disease, development and occurrence of possible (predictable) complications, which can even lead to death.
Prevention of coronary heart disease is indicated for both sick people and healthy people who are at risk of developing the disease. People who have a predisposition to the occurrence of coronary heart disease include those who have at least 1 of the unchangeable and 1-2 of the modifiable causes. If there are more than two reasons, both changeable and unchangeable, then the risk of disease increases. At the same time, people who have even a minimal risk of coronary heart disease and who have crossed the age of 40 should not neglect regular preventive visits to a cardiologist.
Patients diagnosed with coronary heart disease are shown non-drug treatment, which is a complete or partial elimination of causes that can be changed (withdrawal of nicotine, increased physical activity, rationalization of diet, refusal of hormonal contraceptives, etc.) or adjusted (normalization pressure, lowering cholesterol in the blood, etc.).
Prevention of coronary heart disease can also be characterized as improving quality of life. It's no secret that with such bad habits as overeating and poor nutrition, a sedentary lifestyle, smoking and excessive alcohol consumption, a person is simply doomed to the occurrence of various abnormalities, the appearance of diseases that can subsequently become chronic. It is important to understand that prevention of coronary heart disease is necessary and at the same time publicly available.
Quitting nicotine
It is known that smoking, incl. and passive smoking (inhalation of tobacco smoke) is the cause of a wide variety of diseases. Smoking has the most negative effect on the cardiovascular system. Smoking depletes the blood, reduces the oxygen content in the blood, promotes thrombosis and the appearance of atherosclerotic plaques. Inhaled nicotine and carbon monoxide increases pressure in blood vessels and contributes to metabolic disorders. The tars contained in nicotine smoke provoke the heart muscle to contract faster and have an antispasmodic effect on blood vessels. It is important to know that the risk of death for a smoker is 5 times higher than for a non-smoker.
Avoiding excessive alcohol consumption
Alcohol consumption should be kept to a minimum. The alcohol consumption limit for men is 30 grams. and for women 20 gr. translated into pure alcohol.
Normalization of nutrition
It is necessary to reduce blood cholesterol, to reduce body weight, and also to normalize blood pressure. You can normalize your diet without going to extremes (vegetarianism, fasting, etc.). Normal nutrition is when a harmonious balance is established between calories consumed and calories burned. This type of nutrition does not allow the body to accumulate excess fat tissue. Correct balanced diet also does not lead to an increase in cholesterol levels in the blood. Limiting high-calorie, fatty foods, increasing the consumption of vegetable fats and foods, fresh fruits and vegetables allows the body to remove excess cholesterol. Reducing table salt consumption per day to 4 grams. makes it possible to reduce blood pressure to 6 mmHg. Also, you should definitely drink clean, non-chlorinated water - up to two liters per day.
Increasing physical activity
This system of measures is necessary to strengthen the heart muscle, improve the overall tone of the body and to reduce excess body weight. Affordable and easy physical activity - walking, jogging, cycling, swimming, skiing, as well as exercise in gyms - are recommended for everyone without exception, including people with disabilities. initial stage coronary heart disease.
Improvement of psycho-emotional background
Regular visits to the cardiologist. A competent and attentive approach to one’s own health, periodic visits to a cardiologist if there is a risk of coronary heart disease (based on an assessment of the existing causes of the disease), when identifying the very first and minor symptoms of the disease, can not only reduce the risk of occurrence, but also completely avoid the disease .
Risk factors and prevention
Risk factors are any predisposing factors that increase the likelihood of developing or worsening a disease. In Europe and the USA, there are specially developed scales for assessing cardiovascular risk, the main ones being the Framingham scale and the SCORE scale. They make it possible to predict the risk of a heart attack or other heart damage in the next 10 years with an accuracy of several percent. To some extent, these scales are applicable to other countries, but only after careful calibration and modification. No such scale has been developed for Russia.
Risk factors for coronary heart disease are fundamentally divided into removable and irreducible.
Unavoidable risk factors:
- Age - more than 40 years
- Gender - men, as well as older women after menopause, are at the greatest risk.
- Heredity - the presence of relatives who died from heart disease, as well as genetic mutations detected by modern screening methods.
Avoidable risk factors:
- Smoking
- High blood pressure
- Increased blood cholesterol
- Diabetes mellitus or high blood sugar
- Poor nutrition
- Overweight and Obesity
- Low physical activity
- Alcohol abuse
The main task of preventing the development of coronary heart disease is to eliminate or minimize the magnitude of those risk factors for which this is possible. To do this, even before the first symptoms appear, it is necessary to adhere to recommendations for lifestyle modification.
Prevention
Lifestyle modification:
- To give up smoking. Complete cessation of smoking, including passive smoking. The overall risk of mortality for those who quit smoking is halved within two years. After 5 - 15 years, it levels out with the risk of those who have never smoked. If you cannot cope with this task on your own, contact a specialist for advice and help.
- Physical activity. All patients with coronary artery disease are recommended to engage in daily physical activity at a moderate pace, such as walking for at least 30 minutes a day, home activities such as cleaning, gardening, and walking from home to work. If possible, endurance training is recommended 2 times a week. Patients with high level risk (for example, after a heart attack or with heart failure) need to develop an individual physical rehabilitation program. It must be adhered to throughout your life, periodically changing on the recommendation of a specialist.
- Diet. The goal is to optimize nutrition. It is necessary to reduce the amount of solid animal fats, cholesterol, and simple sugars. Reduce sodium (table salt) intake. Reduce the total calorie intake, especially if you are overweight. To achieve these goals, you must adhere to the following rules:
- Eliminate or limit as much as possible the consumption of any animal fat: lard, butter, fatty meat.
- Limit (or better yet completely eliminate) fried foods.
- Limit eggs to 2 per week or less.
- Reduce table salt consumption to 5 grams per day (salt in a plate), and in patients with hypertension to 3 or less grams per day.
- Limit confectionery products, pastries, cakes, etc. as much as possible.
- Increase your consumption of grains, as minimally processed as possible.
- Increase the amount of fresh vegetables and fruits.
- Eat sea fish at least three times a week instead of meat.
- Include omega-3 fatty acids (ocean fish, fish oil) in your diet.
This diet has a high protective effect for blood vessels and prevents further development atherosclerosis.
Weight loss. The goals of the weight loss program for coronary artery disease are to achieve a body mass index in the range of 18.5 - 24.9 kg/m2 and an abdominal circumference of less than 100 cm in men and less than 90 cm in women. To achieve these indicators, it is recommended to increase physical activity, reduce calorie intake, and, if necessary, develop an individual weight loss program and stick to it. At the first stage, it is necessary to reduce the weight by at least 10% of the original and maintain it.
In case of severe obesity, it is necessary to consult a specialist nutritionist and endocrinologist.
Reduce alcohol consumption. According to the latest WHO recommendations, the amount of alcohol consumed should not exceed one bottle of dry wine per week.
Monitoring key indicators
Arterial pressure. If it is within normal limits, you need to check it twice a year. If your blood pressure is elevated, you should take measures as recommended by your doctor. Very often, long-term use of blood pressure-lowering medications is required. The target blood pressure level is less than 140/90 mmHg in people without underlying medical conditions, and less than 130/90 in people with diabetes or kidney disease.
Cholesterol level. An annual screening should include a blood test for cholesterol. If it is elevated, it is necessary to begin treatment on the recommendation of a doctor.
Blood sugar. It is necessary to monitor blood sugar levels especially carefully if you have diabetes or are prone to it; in such cases, constant supervision by an endocrinologist is necessary.
Coronary heart disease is a disease that is a circulatory disorder of the myocardium. It is caused by a lack of oxygen, which is carried through the coronary arteries. Manifestations of atherosclerosis prevent its entry: narrowing of the lumens of blood vessels and the formation of plaques in them. In addition to hypoxia, that is, lack of oxygen, tissues are deprived of some of the beneficial nutrients necessary for the normal functioning of the heart.IHD is one of the most common diseases that causes sudden death. It is much less common among women than among men. This is due to the presence in the body of representatives of the fairer sex of a number of hormones that prevent the development of vascular atherosclerosis. With the onset of menopause, hormonal levels change, so the possibility of developing coronary artery disease increases sharply.
What it is?
Coronary heart disease is a lack of blood supply to the myocardium (heart muscle).
The disease is very dangerous - for example, with acute development, coronary heart disease immediately leads to myocardial infarction, which causes death in middle-aged and elderly people.
Causes and risk factors
The vast majority (97-98%) of clinical cases of coronary artery disease are caused by atherosclerosis of the coronary arteries of varying severity: from slight narrowing of the lumen by atherosclerotic plaque to complete vascular occlusion. With 75% coronary stenosis, heart muscle cells react to the lack of oxygen, and patients develop angina pectoris.
Other causes of IHD are thromboembolism or spasm of the coronary arteries, which usually develop against the background of an existing atherosclerotic lesion. Cardiospasm aggravates the obstruction of the coronary vessels and causes manifestations of coronary heart disease.
Factors contributing to the occurrence of IHD include:
- Hyperlipidemia - promotes the development of atherosclerosis and increases the risk of coronary heart disease by 2-5 times. The most dangerous in terms of the risk of coronary heart disease are hyperlipidemia types IIa, IIb, III, IV, as well as a decrease in the content of alpha lipoproteins.
- Arterial hypertension - increases the likelihood of developing coronary artery disease by 2-6 times. In patients with systolic blood pressure = 180 mmHg. Art. and higher, coronary heart disease occurs up to 8 times more often than in hypotensive patients and people with normal blood pressure.
- Smoking - according to various sources, smoking cigarettes increases the incidence of coronary artery disease by 1.5-6 times. Mortality from coronary heart disease among men 35-64 years old who smoke 20-30 cigarettes daily is 2 times higher than among non-smokers of the same age category.
- Physical inactivity and obesity - physically inactive people have a 3 times greater risk of developing coronary artery disease than people leading an active lifestyle. When physical inactivity is combined with excess body weight, this risk increases significantly.
- Diabetes mellitus, incl. latent form, increases the risk of coronary heart disease by 2-4 times.
Factors that pose a threat to the development of IHD should also include family history, male gender, and elderly age patients. When several predisposing factors are combined, the risk of developing coronary heart disease increases significantly. The causes and rate of development of ischemia, its duration and severity, the initial state of the individual’s cardiovascular system determine the occurrence of one or another form of coronary heart disease.
Signs of IHD
The disease in question can occur quite secretly, so it is recommended to pay attention to even minor changes in the functioning of the heart. Alarming symptoms are:
- periodic feeling of lack of air;
- feeling of anxiety for no apparent reason;
- general weakness;
- periodic chest pain that can radiate to the arm, shoulder blade or neck;
- feeling of tightness in the chest;
- burning or heaviness in the chest;
- nausea and vomiting of unknown etiology.

Symptoms of coronary heart disease
IHD is the most extensive heart pathology and has many forms.
- Angina pectoris. The patient develops pain or discomfort behind the sternum, in the left half chest, heaviness and feeling of pressure in the area of the heart - as if something heavy had been placed on the chest. In the old days they said that a person has “angina pectoris.” The pain can be different in nature: pressing, squeezing, stabbing. It can give (radiate) to left hand, under the left shoulder blade, lower jaw, stomach area and is accompanied by the appearance of severe weakness, cold sweat, and a feeling of fear of death. Sometimes during exertion it is not pain that occurs, but a feeling of lack of air that goes away with rest. The duration of an angina attack is usually several minutes. Since pain in the heart area often occurs when moving, a person is forced to stop. In this regard, angina pectoris is figuratively called “window shopping disease” - after a few minutes of rest, the pain usually goes away.
- Myocardial infarction. A severe and often disabling form of ischemic heart disease. With myocardial infarction, severe, often tearing, pain occurs in the region of the heart or behind the sternum, radiating to the left shoulder blade, arm, and lower jaw. The pain lasts more than 30 minutes; when taking nitroglycerin, it does not go away completely and only decreases for a short time. There is a feeling of lack of air, cold sweat, severe weakness, decreased blood pressure, nausea, vomiting, and a feeling of fear. Taking nitro medications does not help. A section of the heart muscle deprived of nutrition becomes dead, loses strength, elasticity and ability to contract. And the healthy part of the heart continues to work with maximum tension and, contracting, can rupture the dead area. It is no coincidence that a heart attack is colloquially referred to as a heart rupture! As soon as a person in this state makes even the slightest physical effort, he finds himself on the verge of death. Thus, the point of treatment is to ensure that the rupture site heals and the heart is able to continue to function normally. This is achieved both with the help of medications and with the help of specially selected physical exercises.
- Sudden cardiac or coronary death is the most severe of all forms of coronary artery disease. It is characterized by high mortality. Death occurs almost instantly or within the next 6 hours from the onset of an attack of severe chest pain, but usually within an hour. The causes of such a cardiac catastrophe are various kinds arrhythmias, complete blockage of the coronary arteries, severe electrical instability of the myocardium. The provoking factor is alcohol intake. As a rule, patients do not even know that they have coronary artery disease, but they have many risk factors.
- Heart failure. Heart failure is manifested by the inability of the heart to provide sufficient blood flow to the organs due to a decrease in contractile activity. The basis of heart failure is a violation of the contractile function of the myocardium, both due to its death during a heart attack, and due to disturbances in the rhythm and conductivity of the heart. In any case, the heart contracts inadequately and its function is unsatisfactory. Heart failure manifests itself as shortness of breath, weakness during exercise and at rest, swelling of the legs, enlarged liver and swelling of the neck veins. The doctor may hear wheezing in the lungs.
- Heart rhythm and conduction disorders. Another form of IHD. It has a large number various types. They are based on a violation of the conduction of impulses through the conduction system of the heart. It manifests itself as sensations of interruptions in the work of the heart, a feeling of “fading”, “bubbling” in the chest. Disturbances in heart rhythm and conduction can occur under the influence of endocrine and metabolic disorders, during intoxication and drug exposure. In some cases, arrhythmias can occur due to structural changes in the conduction system of the heart and myocardial diseases.
Diagnostics
First of all, the diagnosis of coronary artery disease is carried out on the basis of the patient’s sensations. Most often they complain of burning and pain in the chest, shortness of breath, increased sweating, and swelling, which is a clear sign of heart failure. The patient experiences weakness, heartbeat and rhythm disturbances. It is mandatory to perform electrocardiography if ischemia is suspected.
Echocardiography is a research method that allows you to assess the condition of the myocardium, determine muscle contractile activity and blood flow. Blood tests are performed. Biochemical changes can reveal coronary heart disease. Carrying out functional tests involves physical activity on the body, for example, walking up the stairs or doing exercises on a machine. In this way, heart pathologies can be detected in the early stages.
How to treat IHD?
First of all, the treatment of coronary heart disease depends on the clinical form. For example, although some are used for angina and myocardial infarction general principles treatment, however, treatment tactics, selection of activity regimens and specific medications may differ radically. However, there are some general directions, important for all forms of IHD.
Drug treatment
There are a number of groups of drugs that may be indicated for use in one form or another of coronary artery disease. In the USA there is a formula for the treatment of coronary artery disease: “A-B-C”. It involves the use of a triad of drugs, namely antiplatelet agents, β-blockers and cholesterol-lowering drugs.
- β-blockers. Due to their effect on β-arenoceptors, adrenergic blockers reduce the heart rate and, as a result, myocardial oxygen consumption. Independent randomized studies confirm an increase in life expectancy when taking beta-blockers and a decrease in the incidence of cardiovascular events, including recurrent ones. Currently, it is not advisable to use the drug atenolol, since according to randomized trials it does not improve the prognosis. β-blockers are contraindicated in case of concomitant pulmonary pathology, bronchial asthma, COPD. Below are the most popular β-blockers with proven properties of improving the prognosis of coronary artery disease.
- Antiplatelet agents. Antiplatelet agents prevent the aggregation of platelets and red blood cells, reduce their ability to glue and adhere to the vascular endothelium. Antiplatelet agents facilitate the deformation of red blood cells when passing through capillaries and improve blood fluidity.
- Fibrates. They belong to the class of drugs that increase the antiatherogenic fraction of lipoproteins - HDL, with a decrease in which mortality from coronary artery disease increases. Used to treat dyslipidemia IIa, IIb, III, IV, V. They differ from statins in that they mainly reduce triglycerides and can increase the HDL fraction. Statins primarily reduce LDL and do not have a significant effect on VLDL and HDL. Therefore, for maximum effective treatment macrovascular complications require a combination of statins and fibrates.
- Statins. Cholesterol-lowering drugs are used to reduce the rate of development of existing atherosclerotic plaques and prevent the formation of new ones. Proven positive influence on life expectancy, these drugs also reduce the frequency and severity of cardiovascular events. The target cholesterol level in patients with coronary artery disease should be lower than in persons without coronary artery disease and equal to 4.5 mmol/l. The target LDL level in patients with coronary artery disease is 2.5 mmol/l.
- Nitrates. Drugs in this group are derivatives of glycerol, triglycerides, diglycerides and monoglycerides. The mechanism of action is the influence of the nitro group (NO) on the contractile activity of vascular smooth muscles. Nitrates predominantly act on the venous wall, reducing the preload on the myocardium (by dilating the vessels of the venous bed and deposition of blood). Side effect nitrates are a reduction in blood pressure and headaches. Nitrates are not recommended for use if blood pressure is below 100/60 mmHg. Art. In addition, it is now reliably known that taking nitrates does not improve the prognosis of patients with coronary artery disease, that is, it does not lead to an increase in survival, and are currently used as a drug to relieve the symptoms of angina pectoris. Intravenous drip administration of nitroglycerin can effectively combat the symptoms of angina pectoris, mainly against the background of high blood pressure numbers.
- Lipid-lowering drugs. The effectiveness of complex therapy for patients suffering from coronary heart disease using policosanol (20 mg per day) and aspirin (125 mg per day) has been proven. As a result of therapy, there was a persistent decrease in LDL levels, a decrease in blood pressure, and normalization of weight.
- Diuretics. Diuretics are designed to reduce the load on the myocardium by reducing the volume of circulating blood due to the accelerated removal of fluid from the body.
- Anticoagulants. Anticoagulants inhibit the appearance of fibrin filaments, they prevent the formation of blood clots, help stop the growth of existing blood clots, and enhance the effect of endogenous enzymes that destroy fibrin on blood clots.
- Loop diuretics. Reduce the reabsorption of Na+, K+, Cl- in the thick ascending part of the loop of Henle, thereby reducing the reabsorption (reabsorption) of water. They have a fairly pronounced, rapid effect and are usually used as drugs. emergency assistance(for forced diuresis).
- Antiarrhythmic drugs. Amiodarone belongs to group III antiarrhythmic drugs and has a complex antiarrhythmic effect. This drug acts on the Na+ and K+ channels of cardiomyocytes, and also blocks α- and β-adrenergic receptors. Thus, amiodarone has antianginal and antiarrhythmic effects. According to randomized clinical trials, the drug increases the life expectancy of patients who regularly take it. When taking tablet forms of amiodarone, the clinical effect is observed after approximately 2-3 days. The maximum effect is achieved after 8-12 weeks. This is due to the long half-life of the drug (2-3 months). In this regard, this drug is used for the prevention of arrhythmias and is not an emergency treatment.
- Angiotensin-converting enzyme inhibitors. By acting on the Angiotensin-converting enzyme (ACE), this group of drugs blocks the formation of angiotensin II from angiotensin I, thus preventing the effects of angiotensin II, that is, leveling vasospasm. This ensures that target blood pressure levels are maintained. Drugs in this group have nephro- and cardioprotective effects.
Other treatments for ischemic heart disease
Other non-drug treatments:
- Hirudotherapy. It is a treatment method based on the use of the antiplatelet properties of leech saliva. This method is an alternative and has not been clinically tested to meet the requirements evidence-based medicine. Currently used relatively rarely in Russia, it is not included in the standards of provision medical care for ischemic heart disease, it is used, as a rule, at the request of patients. Potential beneficial effects of this method include the prevention of blood clots. It is worth noting that when treated according to approved standards, this task is performed using heparin prophylaxis.
- Stem cell treatment. When stem cells are introduced into the body, it is expected that the pluripotent stem cells that enter the patient’s body will differentiate into the missing cells of the myocardium or vascular adventitia. Stem cells actually have this ability, but they can turn into any other cell in the human body. Despite numerous statements by supporters of this method of therapy, it is still far from practical application in medicine, and there are no clinical studies that meet the standards of evidence-based medicine that would confirm the effectiveness of this technique. WHO notes this method as promising, but does not yet recommend it for practical use. In the vast majority of countries in the world, this technique is experimental and is not included in the standards of medical care for patients with coronary artery disease.
- Shock wave therapy method. Exposure to low power shock waves leads to myocardial revascularization. An extracorporeal source of focused acoustic wave allows remote influence on the heart, causing “therapeutic angiogenesis” (vascular formation) in the zone of myocardial ischemia. Exposure to UVT has a double effect - short-term and long-term. First, the vessels dilate and blood flow improves. But the most important thing begins later - new vessels appear in the affected area, which provide long-term improvement. Low-intensity shock waves cause shear stress in the vascular wall. This stimulates the release of vascular growth factors, triggering the growth of new vessels that feed the heart, improving myocardial microcirculation and reducing angina. The results of such treatment are theoretically a decrease in the functional class of angina, an increase in exercise tolerance, a decrease in the frequency of attacks and the need for medications.
- Quantum therapy. It is a therapy using laser radiation. The effectiveness of this method has not been proven, and no independent clinical study has been conducted. Equipment manufacturers claim that quantum therapy is effective for almost all patients. Drug manufacturers report studies showing the low effectiveness of quantum therapy. In 2008, this method is not included in the standards of medical care for coronary artery disease; it is carried out mainly at the expense of patients. It is impossible to assert the effectiveness of this method without an independent open randomized trial.

Nutrition for IHD
The menu of a patient diagnosed with coronary heart disease should be based on the principle of rational nutrition, balanced consumption of foods with a low content of cholesterol, fat and salt.
It is very important to include the following products in the menu:
- red caviar, but not in large quantities - maximum 100 grams per week;
- seafood;
- any vegetable salads with vegetable oil;
- lean meats - turkey, veal, rabbit;
- skinny varieties of fish - pike perch, cod, perch;
- fermented milk products - kefir, sour cream, cottage cheese, fermented baked milk with a low fat content;
- any hard and soft cheeses, but only unsalted and mild;
- any fruits, berries and dishes made from them;
- yolks chicken eggs– no more than 4 pieces per week;
- quail eggs - no more than 5 pieces per week;
- any porridge, except semolina and rice.
It is necessary to eliminate or significantly reduce the use of:
- meat and fish dishes, including broths and soups;
- butter and confectionery products;
- Sahara;
- dishes made from semolina and rice;
- animal by-products (brains, kidneys, etc.);
- spicy and salty snacks;
- chocolate;
- cocoa;
- coffee.
If you have diagnosed coronary heart disease, you need to eat fractionally - 5-7 times a day, but in small portions. If you are overweight, then you definitely need to get rid of it - this is a heavy burden on the kidneys, liver and heart.
Traditional methods of treating coronary artery disease
To treat the heart, traditional healers have compiled a lot of different recipes:
- For a liter of honey, take 10 lemons and 5 heads of garlic. Lemons and garlic are crushed and mixed with honey. The composition is kept for a week in a dark, cool place, after infusion, take four teaspoons once a day.
- Hawthorn and motherwort (1 tablespoon each) are placed in a thermos and filled with boiling water (250 ml). After a couple of hours, the product is filtered. How to treat cardiac ischemia? It is necessary to drink 2 tbsp half an hour before breakfast, lunch and dinner. spoons of infusion. It is advisable to additionally brew a rosehip decoction.
- Mix 500 g of vodka and honey and heat until foam forms. Take a pinch of motherwort, marsh cudweed, valerian, knotweed, and chamomile. Brew the herb, let it sit, strain and mix with honey and vodka. Take in the morning and evening, first a teaspoon, after a week - a tablespoon. The course of treatment is one year.
- Mix a spoonful of grated horseradish and a spoonful of honey. Take one hour before meals and drink water. The course of treatment is 2 months.
Facilities traditional medicine It will help if you follow two principles - regularity and strict adherence to the recipe.
Surgery
Under certain parameters of coronary heart disease, indications arise for coronary bypass surgery - an operation in which the blood supply to the myocardium is improved by connecting the coronary vessels below the site of their lesion with external vessels. The best known is coronary artery bypass grafting (CABG), in which the aorta is connected to segments of the coronary arteries. For this purpose, autografts (usually the great saphenous vein) are often used as shunts.
It is also possible to use balloon dilatation of blood vessels. During this operation, a manipulator is inserted into the coronary vessels through a puncture of an artery (usually the femoral or radial), and using a balloon filled with a contrast agent, the lumen of the vessel is expanded; the operation is, in essence, bougienage of the coronary vessels. Currently, “pure” balloon angioplasty without subsequent stent implantation is practically not used, due to its low effectiveness in the long term. If the medical device is moved incorrectly, it can result in death.

Prevention and lifestyle
To prevent the development of the most severe forms of coronary heart disease, you need to follow only three rules:
- Leave your bad habits in the past. Smoking and drinking alcoholic beverages is like a blow that will definitely lead to a worsening of the condition. Even an absolutely healthy person does not get anything good from smoking and drinking alcohol, let alone a diseased heart.
- Move more. Nobody talks about setting Olympic records, but giving up the car, public transport and an elevator in favor of walking is necessary. You can’t immediately load your body with kilometers of roads traveled - let everything be within reason. To ensure that physical activity does not cause a worsening of the condition (and this happens with ischemia!), be sure to consult with your doctor about the correctness of the exercises.
- Take care of your nerves. Try to avoid stressful situations, learn to react calmly to troubles, and do not give in to emotional outbursts. Yes, it’s hard, but this is the tactic that can save lives. Consult your doctor about the use of sedative medications or infusions. medicinal plants with a calming effect.
Coronary heart disease is not only periodic pain, long-term disruption of coronary circulation leads to irreversible changes in the myocardium and internal organs, and sometimes even to death. Treatment of the disease is long-term, sometimes requiring lifelong medication. Therefore, it is easier to prevent heart disease by introducing some restrictions into your life and optimizing your lifestyle.